Graham Davies’ Survival Story
Pseudomyxoma Peritonei (PMP)
This is my personal account of my battle with a very rare form of cancer known as Pseudomyxoma Peritonei (PMP). It’s written in the form of a diary, which I updated regularly. I hope my story will give encouragement and support to fellow-sufferers.
Contents
- First symptoms: 2003-2005
- More symptoms: September 2005
- I am diagnosed with cancer: December 2005 to February 2006
- Major surgery: 1 March 2006
- The beginning of my recovery: March 2006
- Diagnosis of Deep Vein Thrombosis (DVT): 2 April 2006
- My disease is identified as Pseudomyxoma Peritonei (PMP): 26 April 2006
- We miss our daughter’s wedding: 8 May 2006
- Holiday weekend in Brussels: 1-4 June 2006
- Post-op MRI Scan: 9 June 2006
- The summer of 2006: birth of our second granddaughter
- Visit to Basingstoke and North Hampshire Hospital: 4 October 2006
- Colonoscopy and CT scan: 1 November 2006
- Visit to Basingstoke and North Hampshire Hospital: 3 January 2007
- First anniversary of my operation: 1 March 2007
- Visit to Basingstoke and North Hampshire Hospital: 4 April 2007
- Re-run of our daughter’s wedding: May 2007
- My 65th birthday celebration: 2 June 2007
- Enjoying the summer of 2007
- CT Scan: 7 August 2007
- Colonoscopy: 8 November 2007
- Skiing holiday: January 2008
- CT scan: 19 February 2008
- Second anniversary of my operation: 1 March 2008
- My 66th birthday celebration: 2 June 2008
- Interview with my oncologist: 11 August 2008
- Our Ruby Wedding anniversary: 24 August 2008
- Birth of our grandson: 23 December 2008
- CT scan: 3 February 2009
- Third anniversary of my operation: 1 March 2009
- Looking back on 2009
- The start of 2010
- Fourth anniversary of my operation: 1 March 2010
- The summer of 2010
- October 2010: Laparoscopy
- November 2010: Interview with my oncologist
- February 2011: Interview with my oncologist
- Fifth anniversary of my operation: 1 March 2011
- CT scan: 18 April 2011
- The summer of 2011
- November 2011: Interview with Mr Cecil
- February 2012: CT scan
- Sixth anniversary of my operation: 1 March 2012
- Interview with Mr Cecil, 28 March 2012
- Wexham Park Hospital, 3-14 April 2012
- Interview with Dr Brown, oncologist, 18 April 2012
- Interview with Dr Rees, oncologist, 8 May 2012
- Macmillan Cancer Support, 25-28 May 2012
- Thames Valley Hospice, 31 May to 2 June 2012: 70th Birthday BBQ
- Thames Valley Hospice, 19 June 2012
- My diet
- Concluding thoughts
- Support of family and friends
- Useful links relating to PMP and other survivors’ stories
First symptoms: 2003-2005
I have always led an active life. I have travelled all over the world, and I enjoy walking, swimming, playing golf and skiing. As a younger man I used to scuba-dive. I have had a successful career as a university teacher – see my personal wiki: http://grahamdavies.wikispaces.com
I have rarely been ill, apart from suffering from a mild form of ulcerative colitis, which was first diagnosed in the early 1970s when I was around 30 years of age. The ulcerative colitis has never been a major problem. It has been successfully controlled by medication. It would flare up only occasionally and become an annoyance – that is until the summer of 2003. I then began to suffer a series of major flare-ups, which led to my being referred by my GP to a gastro-intestinal consultant at Wexham Park Hospital, Slough, in October 2003. A colonoscopy in January 2004 revealed that the colitis was more active than usual, and I was prescribed new medications, Asacol (long-term medication) and Prednisolone (a “quick-fix” steroid which I took for about a month), that brought the flare-ups under control.
In the summer of 2003 I also developed an allergy to shellfish. I had eaten prawns, mussels, crabs and lobsters all my life without ill-effects, but now even a single prawn would cause my lips and face to swell up and hives to appear all over my body. I also became extremely breathless. I was referred by my GP to an allergy consultant, who advised me not to eat shellfish and prescribed an Epipen for emergencies. Curiously, the allergy has now completely disappeared – see Concluding thoughts (below).
Following a skiing holiday in January 2005, I developed a persistent cough. My GP arranged for an xray examination, but this revealed nothing sinister. Following further tests at my GP’s surgery, it was concluded in March 2005 that I had asthma, and I was prescribed a preventative inhaler – which seemed to work. Curiously, the cough has now completely disappeared – see Concluding thoughts (below).
Around this time I was also beginning to develop what I thought to be typical old man’s symptoms, i.e. a frequent need to empty my bladder, which I thought might indicate prostate problems, but an examination by my GP and a PSA blood test indicated that my prostate was in good order, so no further action was taken. Read on…
More symptoms: September 2005
In August 2005 I experienced severe pain in my bladder, which was identified by my GP’s locum as cystitis and I was prescribed a course of antibiotics. The antibiotics relieved the symptoms, but there were still traces of blood in my urine, which my GP identified on a follow-up visit. My GP felt my abdomen and looked puzzled, as my bladder appeared to be very enlarged and extending right up to my navel. He therefore immediately contacted our local hospital to arrange for an ultrasound scan (September 2005) and referred me to a consultant urologist. The ultrasound showed evidence that I could not fully empty my bladder, which was retaining about 250ml of urine, so something was obviously wrong.
I am diagnosed with cancer: December 2005 to February 2006
I had to wait until 8 December 2005 for an appointment with a consultant urologist, who identified “cysts” around the bladder area – possibly benign, he said. An appointment was made for me to have an immediate MRI scan, which took place on 16 December 2005 at Wexham Park Hospital. I was now becoming extremely anxious, as my father had died of bladder cancer and I wondered if I would suffer the same fate. I got the results of the MRI scan in early January 2006 when I received a telephone call from a consultant surgeon at Wexham Park Hospital, who informed me that there was “something nasty” in my abdomen. An immediate appointment was arranged for a cystoscopy – which involves the insertion of a tiny camera into the bladder under a local anaesthetic. The doctor who conducted the cystoscopy looked puzzled. The inside of my bladder looked OK – I was able to view it on a TV screen – but something appeared to be pressing into the bladder from outside, like a fist pushed into a balloon.
Another appointment with my consultant urologist followed within a few days. He called in a second consultant urologist, who looked at the results of the MRI scan and the cystoscopy and described what he saw as “interesting”. The MRI scan showed a large tumour in my abdomen and it was by now clear that it would have to be removed by surgery. I was about to go on a skiing holiday and asked the two consultants if I should cancel the holiday. They said there was no need to cancel and arranged an appointment for a bone scan and a CT scan to be carried out in early February 2006 just after on my return from my holiday, followed by another appointment with the second consultant urologist and a pre-operative examination.
By now the second consultant urologist was in charge of my fate. He explained to me that I had a very rare form of cancerous tumour and he would lead the surgical team to remove it. He said that the tumour appeared to be emanating from my urachus, the remnant of a tube that extends from the dome of the bladder to the navel and which only has a function prior to one’s birth. I had never heard of the urachus before, and I imagine that most people are unaware of its existence. The tumour was pressing on the outside wall of my bladder, making it difficult for me to pass urine and causing the cystitis-like symptoms I first experienced in August 2005. Half my bladder would have to be removed, the consultant said. I was somewhat alarmed by this, but he said it would not cause me long-term problems. The date for my operation was fixed for 1 March 2006, and I was admitted into Wexham Park Hospital on 28 February 2006.
Major surgery: 1 March 2006
The pre-op procedure was initially a bit alarming. I was visited by the stoma nurse and told that my bladder might have to be removed and that part or all of my colon might have to be removed too. The nurse explained to me that I might – but this was only a remote possibility – end up with two plastic bags fixed to my abdomen to collect urine and excreta. She marked two points on my abdomen where the bags would be fixed if this was necessary.
I was quite calm immediately before the operation. A senior surgeon explained the nature of the operation and the anaesthetist was reassuring, explaining that modern anaesthetics are generally very safe and cause few after-effects. He said that I would be given an epidural in order to minimise the pain following the operation.
The operation took just under four hours. I recall coming round and hearing the voice of a nurse watching over me in the recovery room. My abdomen was completely numb and painless – the epidural was working. I asked the nurse what had been done to me. She said that the tumour had been removed, along with half my bladder. What a relief! No nasty plastic bags, but I had two catheters in my bladder, one of which had been inserted directly into the top of my bladder via a hole bored into my abdomen. The other catheter had been inserted via the “normal” route. I was taken to the intensive treatment unit (ITU) and wired up to lots of different monitors and drips. I was allowed a visit by my wife Sally and our younger daughter Francesca around four hours after the end of my operation. They were fascinated by all the equipment surrounding me and by the tube up my nose (the so-called NG tube – nasal-gastric tube) that went all the way down to my stomach in order to keep it drained and to allow my digestive system to rest. I cannot fault the care I received in the ITU.
On the following morning I was visited by a physiotherapist, who showed me how to cough while holding my abdomen (in order to stop my wound reopening), and said that I would also have to get out of bed, stand up and sit in a chair. I could not believe that I would be able to stand up after all that I had been through, but the physiotherapist was very gentle and patient, and I managed to do what she asked. I was now considered stable enough to be transferred to a general ward.
In the general ward I was connected to an epidural drip, a liquid drip of some sort and a device that could deliver a shot of morphine if I experienced pain. I still had a tube up my nose and two catheters in my bladder. I was not allowed to drink or eat. I had a look at my abdomen. There was a wound about 25 centimetres long, extending from the base of my bladder to a few centimetres about my navel. It was held together by a long row of metal clips, and there was a tube draining off excess blood into a small plastic bag. I was visited by one of the surgeons who helped perform my operation. He was not very helpful, explaining only that the tumour that was removed from my abdomen was “very nasty” and that I could not be considered “cured”. Later on he said the prognosis was not very good. Just what I needed to cheer me up! A junior surgeon was more forthcoming. He said that the tumour had a hard core the size of a tennis ball and a surrounding jelly-like mass almost the size of a football. He said that the operation went very well. The leader of the surgical team, the second consultant urologist whom I saw prior to my operation, visited me, saying only that he had achieved all that he set out to do – again very sketchy information.
It was the clinical nurse who finally told me that my tumour was identified as a mucinous adenocarcinoma of the urachus and that it had spread to my omentum, which is a kind of “apron” that protects the bowels. She summarised the discussions of the surgical team regarding my condition and was generally encouraging, explaining that an appointment would be arranged with Dr Richard Brown, a senior oncologist, following my discharge from hospital and that he would be responsible for my long-term care.
The beginning of my recovery: March 2006
My recovery following the operation started well. I regained my strength quickly and was soon able to take short walks around the ward. I was allowed to drink and eat. The tube in my nose was then removed. But after that it all started to go downhill. I began to hiccup non-stop. I vomited incessantly, and a new tube was inserted into my nose in order to drain my stomach. I began coughing up mucus and blood. An xray of my lungs was taken, but nothing serious was indicated. Antibiotics were prescribed and they appeared to work. But I felt miserable. All the nurses and doctors could say was that the hiccups and the nausea would eventually stop. They were right. After five days of hiccuping and vomiting I awoke from my sleep feeling OK and I was able to take food in liquid form. However, I was now suffering from a potassium deficiency and had to drink a foul-tasting liquid twice a day in order to build up my potassium level again. This took two days and then I switched to bananas, which are a rich natural source of potassium. I was now ravenous. I had lost around 20 pounds in weight – part of which was the tumour – and I was devouring Rich Tea biscuits, bananas and Turkish Delight chocolate day and night as a supplement to the hospital food.
On the plus side, my wound healed very quickly and all the clips were removed in two stages, beginning seven days after the operation. Within 10 days all the tubes, apart from the two catheters, had been removed from my body and I was able to walk around the hospital, often visiting the public WRVS canteen with my visitors. The two catheters were removed two weeks after my operation and two days later I was discharged. I was relieved to be able to go home. But it did not stop there. In the early morning following my first night at home I experienced severe pain in my kidneys. I could not urinate. I was suffering from urine retention and backflow to the kidneys. My half-bladder wasn’t working! My wife Sally rang the hospital, and I was told to get straight to A&E at Wexham Park Hospital. My son-in-law Rob came round to our house and drove me there. A new catheter was inserted into my bladder, and I was readmitted into hospital. The pain in my kidneys stopped almost immediately.
I was kept under observation for another week. In the course of this week I appeared to be doing very well, so much so that I was allowed to go home for one night – complete with catheter and leg bag – and told to return for a final check on the following day. It was great to go home again. Sally phoned our elder daughter Siân and she drove us to our local pub, where we had a meal and a couple of drinks (soft drinks for me). The pub food, good old fish and chips and mushy peas, tasted wonderful! On the following day I returned to the hospital where I underwent a procedure in the theatre that involved filling my bladder with an iodine solution to check it for leaks and to ensure that it was working. It was 100% OK. I spent one more day in hospital. I could urinate again, albeit only around 125ml at a time – but this would improve over the next few weeks. I was discharged on 24 March 2006 and I returned home. I had spent a total of 24 days in hospital.
One week after I was discharged from hospital Sally and I went to see one of the surgeons who operated on me. He was not at all encouraging, saying that the prognosis was not good and “it won’t be years”. Sally, who is a very astute university graduate in philosophy, challenged him to provide the evidence. He turned to his computer, finding just a handful of cases like mine, with very varying survival rates. He pointed to two case studies on his computer: one patient had died just a few months post-op and the other had survived for around 20 years. “What do you do?” Sally asked, “Take the average?” Finally, the surgeon admitted that there was a shortage of data concerning my type of cancer and that it was very difficult to predict how an individual would handle it.
During the last week of my stay in hospital l received two pieces of very sad news:
- A friend of mine in his mid-50s had been admitted, without my knowledge, into the hospital where I had my operation and had died of a heart attack in a ward just along the corridor from my ward.
- My only surviving aunt, aged 95, had had a serious fall and had died.
Both funerals took place the week after I was discharged from hospital, and I was still feeling a bit weak and learning to cope with a much reduced bladder that required frequent visits to the toilet. I could not attend either of the funerals.
Diagnosis of Deep Vein Thrombosis (DVT): 2 April 2006
There was one more setback to my recovery. I was diagnosed with Deep Vein Thrombosis (DVT) on 2 April 2006. I had experienced some pain in walking after the operation, but I dismissed it as a general post-op symptom. By 2 April the pain had become acute and my left leg was very swollen. My son-in-law Tim drove me to Heatherwood Hospital, Ascot, for assessment. DVT was identified in the thigh of my left leg and I was immediately given a course of injections of Fragmin. After the course of injections I was prescribed Warfarin, which thinned my blood, prevented new clots forming and helped the old clot to disperse naturally.
Following the first diagnosis of DVT the area of the clot was scanned regularly by ultrasound to check on its progress, and I had several appointments with different vascular consultants. None of them could not say for certain whether the clot had formed as a result of the surgery or whether it was already there before my operation – as the body sometimes forms clots in reaction to cancer. Anyway, DVT has not been a major problem for me. It has not stopped me doing the things that I enjoy: swimming, walking a mile every day with our greyhound, playing golf, and going on skiing holidays once or twice a year. After the diagnosis in April 2006 I was advised by a senior vascular consultant not to travel by air. As a result, I rediscovered the pleasure of going on driving holidays all over Europe. I now always wear compression socks when I drive on a long journey and I remember to stop at regular intervals and walk around for 10-15 minutes.
Now the good news! In December 2007 I was told by my vascular consultant that the DVT condition had improved and that I could fly short-haul for up to four hours. I had been invited to attend a meeting at a university in Hungary in April 2008, so I booked my first flight for over two years, and in May 2008 my wife Sally and I flew to Valencia for a short holiday combined with a business trip. Finally, in June 2008, one of my vascular consultants told me that I was asymptomatic, that the blood flow in my left thigh was nearly normal and that I could travel long-haul by air if I wished – taking the usual precautions, i.e. wearing compression socks, moving around as much as possible, drinking plenty of non-alcoholic fluids and making sure that I sat in a seat with plenty of leg room – which means that most economy seats are out of the question.
My disease is identified as Pseudomyxoma Peritonei (PMP): 26 April 2006
On 26 April 2006 Sally and I had our first interview with Dr Richard Brown, a senior oncologist, at Heatherwood Hospital, Ascot. He was generally very upbeat and encouraging. He was impressed by how fit I looked and said that we were fortunate to live quite near to the Basingstoke and North Hampshire Hospital, to which he would refer me for follow-up scans and consultations. When Dr Brown mentioned the name of this hospital Sally asked him if my disease was a variety of Pseudomyxoma Peritonei (PMP). Sally and I had done a lot of research on the Web, trying to find our more about the mucinous adenocarcinoma tumour that was removed from my abdomen, and Sally had already suspected that it might be a variety of PMP, Basingstoke being one of two UK centres that specialise in treating it. Dr Brown confirmed that I did indeed have a variety of PMP, a rare type of cancer that affects one in a million people.
PMP usually starts in the appendix, and it is often referred to as appendix cancer. In women it can also start in the ovaries. My variety of PMP, however, started in the urachus, the remnant of a tube that extends from the dome of the bladder to the navel while the baby is in the womb. Statistics for urachal PMP are hard to come by as it is a very rare sub-variety of PMP. Estimates suggest that urachal PMP affects about one in 5 million people or even as few as one in 10 million people: see Sugarbaker et al. (2008).
PMP does not act like most cancers. Most cancers spread in three different ways: (i) by invading nearby tissues, (ii) via the bloodstream, (iii) via the lymphatic system. PMP, however, spreads along the internal surfaces within the abdomen, rather than into nearby tissues such as the bowel or liver – although these organs can be involved in the long term. A mucus, a jelly-like substance, is thrown out by the core of the tumour, and this collects in the peritoneum, a kind of lining of the cavity of the abdomen. It may be many years before symptoms of this type of cancer manifest themselves. This is exactly my experience. I just thought that I was developing a “beer belly”. It was only when the tumour began to press upon my bladder that I experienced any painful symptoms. PMP is often referred to as jelly belly.
PMP does not have a very high profile as so few people are affected by it. Even experienced general surgeons may know little about it. The most notable victim of the appendix variety of PMP is Audrey Hepburn. If she had been born around 20 years later, she would probably have benefited from the recent knowledge about this disease that has been gained, and maybe she would have survived. See this article: The Fairest of All: http://tinyurl.com/yhmbprh. See also this extract from the book, Audrey Hepburn: An Elegant Spirit (2003), by her son, Sean Ferrer: http://www.pmpawareness.org/files/audreyhepburn.doc
Dr Brown arranged for an immediate appointment at Reading Hospital for my kidneys to be checked in case I needed chemotherapy and for a post-op MRI scan to take place at Wexham Park Hospital on 9 June 2006. He also wrote to Basingstoke, requesting an appointment for Sally and me to meet Mr Cecil, a senior consultant surgeon who specialises in PMP.
We miss our daughter’s wedding: 8 May 2006
Sally and I were hit by another blow. Our younger daughter Francesca was to be married in Barbados on 8 May 2006 – a special wedding trip. I had the foresight to cancel the flights and hotel reservation for Sally and me when I received confirmation of the date on which I was to be admitted into hospital. It was fortunate that I did so, as I could not have undertaken a long-haul flight: I had DVT and I was still feeling a bit weak. Furthermore I could have lost a lot of money if I had cancelled at the last minute. So we missed our daughter’s wedding. Read my account of the battle I had with my travel insurance company: see my Cautionary Tale.
I became a bit depressed around this time. The initial prognosis I was given following my operation was not optimistic, but I was determined to continue looking forward. For a while I stopped buying new things for myself and I neglected our garden. But then I thought to myself, “This is silly, pull yourself together”, and I went to the garden centre to buy trayloads of summer bedding plants. The exercise I got from tending our garden did me good, and soon we had a lovely display of flowers. I also bought myself a new pair of summer shorts (more expensive than I would normally choose) for playing golf, an expensive shirt and silk tie, and I spent around £750 on new spectacles. Later on, I bought a new satnav device for my car and began to think about driving holidays in Europe. After that, I never looked back. From now on the news was going to be much more optimistic.
Holiday weekend in Brussels: 1-4 June 2006
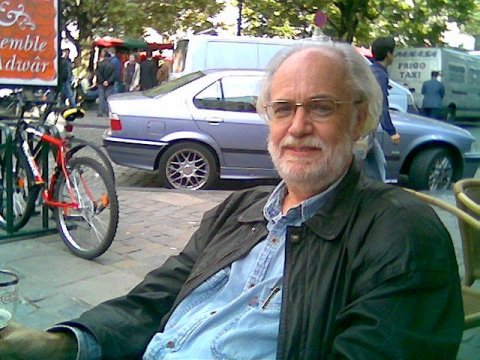
Three months after my operation I was fully active again, doing all the things that I used to do. My half-bladder was functioning more or less normally and I no longer had to get up several times during the night. Sally and I decided to celebrate my 64th birthday on 2 June 2006 by going to Brussels for a long weekend. We decided that expense was no object, so we travelled first class by Eurostar and stayed in the five-star Meridien Hotel. Here is a picture of me enjoying a glass of Leffe in Brussels on my birthday. I felt really fit and well. It was a great weekend.
Post-op MRI Scan: 9 June 2006
My first post-op MRI scan took place at Wexham Park Hospital on 9 June 2006. Sally and I were given the results at Heatherwood Hospital on 23 June 2006. It was good news: no new growth, no signs of the lymph nodes or bones being affected, no visible remnants of the tumour – which compared very favourably with the mess that could be seen in my pre-op MRI scan. It was a beautiful sunny day, which we’ll never forget. Heatherwood Hospital is right opposite Ascot racecourse, and we had a great view of people arriving for Royal Ascot: the men in their morning suits and top hats, the ladies in their elegant dresses and, of course, big hats! Sally and I had a boozy lunch in our local pub to celebrate the positive news.
The summer of 2006: birth of our second granddaughter
The summer I spent at home in 2006 following my operation was beautiful. We had many sunny days. I spent a lot of time lazing around on our garden patio. We had lots of barbecues and I enjoyed taking our greyhound for longer and longer walks in the Berkshire countryside. I swam regularly in the local Holiday Inn pool and I played several rounds of golf. On 2 August 2006 our second granddaughter, Aela, was born, daughter of our elder daughter Siân and son-in-law Tim. Things were looking up. By the end of the summer Sally and I felt it was time for a “proper” holiday, so we decided to spend a two-week driving holiday in Europe – putting my new satnav device to the test – staying for a week in Interlaken, Switzerland, a town that we had visited many times when our two daughters were much younger. This raised the issue of travel insurance again: see my Cautionary Tale. It was a wonderful holiday. We drove down to Switzerland via the Rhineland in Germany, enjoying the wine in Rüdesheim, and returning via France, where we visited the picturesque towns of Colmar in Alsace and Le Touquet on the north coast.
Visit to Basingstoke and North Hampshire Hospital: 4 October 2006
On 4 October 2006 Sally and I had our first interview with Mr Tom Cecil, a senior consultant surgeon who specialises in PMP, at the Basingstoke and North Hampshire Hospital. He was generally very upbeat about my level of fitness, gave us more information about the nature of PMP and talked about possible cures, including the Sugarbaker “shake and bake” operation that is performed at Basingstoke. This is a long, major operation involving the removal of the gallbladder and the spleen, and Hyperthermic Intraperitoneal Chemotherapy (HIPEC), whereby a heated chemo infusion is washed around the abdomen for a hour after the surgical procedures have been completed. It’s a serious operation, often referred to as MOAS (Mother Of All Surgeries), but it has a high success rate and offers a long-term cure.
Colonoscopy and CT scan: 1 November 2006
Mr Cecil arranged for a colonoscopy to be carried out on 1 November 2006 at Wexham Park Hospital and a CT scan of my abdomen to be carried out on 14 November 2006 at Basingstoke. He wrote to Dr Richard Brown, my oncologist, giving his assessment of my situation. Basically, he said, it was a question either of carrying out the operation in the near future or a policy of watch and wait. The results of the colonoscopy were good. I still had a mild form of ulcerative colitis, but there was no evidence of PMP invading the large bowel.
Visit to Basingstoke and North Hampshire Hospital: 3 January 2007
I had to wait until 3 January 2007 for my next interview with Mr Cecil at the Basingstoke and North Hampshire Hospital. The results of my CT scan on 14 November 2006 looked good, he said. There were just two tiny slivers of PMP mucus evident in my abdomen, one near the liver and one just above the bladder. Nothing to be concerned about, Mr Cecil said, but the situation needed to be watched carefully. So I was able to go on my skiing holiday in Austria in January 2007 relatively free from worries. On 26 February 2007 I had an interview with Dr Brown, my oncologist, who had seen the results of the CT scan and who confirmed that it was still a policy of watch and wait.
First anniversary of my operation: 1 March 2007
 It’s one year post-op, and I still feel fit and well, but I still think about the the pessimistic prognosis that “it would not be years”, which Sally and I were given by one of the surgeons who operated on me. Being half-Welsh, I always thought that having an operation on 1 March, St David’s Day, was a good omen.
It’s one year post-op, and I still feel fit and well, but I still think about the the pessimistic prognosis that “it would not be years”, which Sally and I were given by one of the surgeons who operated on me. Being half-Welsh, I always thought that having an operation on 1 March, St David’s Day, was a good omen.
Visit to Basingstoke and North Hampshire Hospital: 4 April 2007
On 4 April 2007 I had another interview with Mr Cecil at the North Hampshire Hospital. He said that it was still a policy of watch and wait and he arranged for a follow-up CT scan to be carried out on 7 August 2007.
Re-run of our daughter’s wedding: May 2007
The biggest disappointment for Sally and me after my operation on 1 March 2006 was that we were unable to attend the wedding of our younger daughter Francesca to Rob in Barbados on 8 May 2006. So we arranged a sort of “re-run” one year on, combining it with the 5th wedding anniversary of our elder daughter Siân and her husband Tim, who were married on 4 May 2002. It was a modest family celebration at Francesca and Rob’s house in Maidenhead – just the six of us and our two granddaughters, Rebecca and Aela. It was a lovely sunny day and Francesca looked gorgeous in her wedding dress.
65th birthday celebration: 2 June 2007
This was to be a summer of celebrations. I became an old age pensioner on 2 June 2007, an event which I decided to celebrate by organising a barbecue for family and friends at our local pub. Around 40 people turned up. It was another lovely sunny day. Here’s a picture of Sally and me in the early evening:

Enjoying the summer of 2007
By now I was determined to make the most out of life. Sally and I took two summer holidays, driving down the Rhine for one week in July and touring Ireland for two weeks in September.
CT Scan: 7 August 2007
The results of the CT scan and the blood test which were carried out on 7 August 2007 at the Basingstoke and North Hampshire Hospital were good. On 19 September 2007 Mr Cecil told me that the slivers of PMP jelly in my abdomen were shrinking and that the sliver above the bladder had actually disappeared. My body appeared to be fighting PMP very effectively. I was told that it would not be necessary for another CT scan to be carried out until August 2008 but I could have an earlier scan if I wished.
On 24 September 2007 I had an interview with Dr Brown at Heatherwood Hospital. He had seen the results of the CT scan carried our on 7 August. He said that my PMP was currently in remission and that he did not need to see me until 22 September 2008. Basically, he was telling me to go away and enjoy life.
Colonoscopy: 8 November 2007
Another routine colonoscopy at Wexham Park Hospital. The results were good. No signs of new growths. I still had mild ulcerative colitis, but I have had no major flare-ups for many months.
Skiing holiday: January 2008
Skiing holiday in Austria, January 2008. The holiday was wonderful. I skiied well, in almost perfect snow conditions: substantial falls of powdery snow on two days and clear blue skies the rest of the time. We were joined by our elder daughter Siân, her husband Tim, our granddaughter Aela, my brother Chris and our sister-in-law Helen – and a few other relatives from Ireland.
CT scan: 19 February 2008
I chose to have another CT scan and blood test carried out at the Basingstoke and North Hampshire Hospital on 19 February 2008. The results were good: my blood was normal and there were no visible signs of PMP fluid or jelly in my abdomen. Yippee! My next follow-up scan and blood test will be February 2009.
Second anniversary of my operation: 1 March 2008
 The date 1 March 2008 is significant. This is the second anniversary of my operation, so the pessimistic prognosis that “it would not be years”, which Sally and I were given following my operation, was wrong. It is years – only two so far, but that’s a good start.
The date 1 March 2008 is significant. This is the second anniversary of my operation, so the pessimistic prognosis that “it would not be years”, which Sally and I were given following my operation, was wrong. It is years – only two so far, but that’s a good start.
My 66th birthday celebration: 2 June 2008
Another birthday! I celebrated my 66th birthday today – a more modest affair than the big bash last year. I feel even fitter than I did this time last year.
Interview with my oncologist: 11 August 2008
My first interview with Dr Brown, my oncologist, for nearly a year. He commented on how fit I looked. He decided it might be a good time to contact the surgeon who operated on me in March 2006 and to notify him that I was doing so well. Next appointment with Dr Brown: one year from now.
Our Ruby Wedding anniversary: 24 August 2008
Two and a half years ago I was not sure that I would reach this important landmark. Today is our Ruby Wedding Anniversary: 40 glorious years! Sally and I celebrated by going on holiday to St Johann in Tirol, Austria, the resort which we visited on our first holiday together in 1966, around a year after we had met. We also took in a festival in Rüdesheim on the Rhine on the way home. We have booked our skiing holiday in St Johann in Tirol, Austria, January 2009.
Birth of our grandson: 23 December 2008
Another cause for celebration: our grandson Joseph came into the world today – grandchild No. 3, joining his sister Rebecca (4) and cousin Aela (2). What a wonderful Christmas present for all the family! The year is certainly ending on a high note and I am really looking forward to our skiing holiday in Austria next month.
CT scan: 3 February 2009
I had my annual CT scan and blood test on 3 February 2009 and got the results on 19 February 2009. There was no evidence of PMP in my abdomen and my blood was normal. Next scan and test in one year from now. Yippee!
Third anniversary of my operation: 1 March 2009
 The date 1 March 2009 is significant. This is the third anniversary of my operation. I have been cancer-free for three years and I have been given the all-clear for a fourth year.
The date 1 March 2009 is significant. This is the third anniversary of my operation. I have been cancer-free for three years and I have been given the all-clear for a fourth year.
Looking back on 2009
A good year for my health – no recurrences of PMP – but a bad year in other ways. The main thing that I remember about 2009 was the dreadful summer: rain, rain, wind, rain. In addition, three of our kitchen appliances had to be replaced at great expense, there were big bills for repairs to our cars, both sons-in-law were made redundant, and our daughter Siân, our son-in-law Tim and our granddaughter Aela were stranded in France when their car broke down. Finally, in mid-June, our greyhound Swifty suddenly went lame in one hind leg. After six weeks of visits to the vet – and huge bills – it was discovered that Swifty had aggressive bone cancer and he had to be put to sleep on 31 July, aged 10 years and 8 months. We both miss him, especially my wife Sally, for whom he was a wonderful companion while I was in hospital in March 2006.
Now the good news: I reached the age of 67 on 2 June and I am still 100% fighting fit. Our elder granddaughter, Rebecca, celebrated her 5th birthday in June, and our younger granddaughter, Aela, celebrated her 3rd birthday in August. We intended to wait a few weeks before we adopted a new greyhound, but on Sunday, 9 August, we went to a barbecue at the Greyhound Welfare kennels in Surrey and a handsome silver brindle hound called Brett caught our eye. The manager of the kennels said that we could take him home straight away. Well, that finalised it. Here is his photo, together with photos of our other dear departed hounds: Greyhounds.
In September, Sally and I enjoyed a holiday in Spain, combining it with a conference at which I ran a workshop for language teachers interested in learning about Second Life. The autumn was gorgeous, Brett settled in well into his new home and I enjoyed many long walks with him in the beautiful Berkshire countryside.
Just before Christmas we took our two grandaughters to see Santa, with real reindeer, at the local department store, and we celebrated our grandson Joseph’s first birthday.
The start of 2010
We have just returned from a wonderful skiing holiday in Austria, 16-30 January. We travelled out with our daughter Siân, son-in-law Tim, granddaughter Aela, my brother Chris and sister-in-law Helen. They were with us for the first week, and Sally and I stayed on for a second week. I skied well: 11 days without a single fall and no bruises or broken bones – just weary legs. Aela spent a few days in ski school and made excellent progress – start ’em young!
Fourth anniversary of my operation: 1 March 2010
 It’s four years post-op, and I still feel great. I have put the pessimistic prognosis that I was given in 2006 behind me. But on 3 March I went to Basingstoke Hospital, where my wife and I had a long chat with Mr Cecil. The annual CT scan carried out on 4 February showed evidence of a small amount of new growth of a 2cm rind of mucin on the surface of my liver and spleen, and a few small nodules elsewhere. The advice I was given was to have another CT scan in 6 months – no hurry, as PMP is a very slow grower. Not the outcome I wanted, but I feel reassured and positive after seeing Mr Cecil and receiving a letter in which he referred to me being “very fit” and also mentioned the high success rate of the Sugarbaker operation if it proves necessary. At least I am not completely in the dark as I was four years ago – which was scary. I am now much better informed, I know what to expect and my general feeling is that I can handle this.
It’s four years post-op, and I still feel great. I have put the pessimistic prognosis that I was given in 2006 behind me. But on 3 March I went to Basingstoke Hospital, where my wife and I had a long chat with Mr Cecil. The annual CT scan carried out on 4 February showed evidence of a small amount of new growth of a 2cm rind of mucin on the surface of my liver and spleen, and a few small nodules elsewhere. The advice I was given was to have another CT scan in 6 months – no hurry, as PMP is a very slow grower. Not the outcome I wanted, but I feel reassured and positive after seeing Mr Cecil and receiving a letter in which he referred to me being “very fit” and also mentioned the high success rate of the Sugarbaker operation if it proves necessary. At least I am not completely in the dark as I was four years ago – which was scary. I am now much better informed, I know what to expect and my general feeling is that I can handle this.
The summer of 2010
All in all, it’s been a good and eventful summer. I celebrated my 68th birthday on 2 June 2010 and I continue to enjoy a high level of physical fitness.
Our new greyhound, Brett, has settled in well. He’s a big lovable boy and great with our grandchildren. He won first prize in his class (dogs aged 5 and under) at the Wimbledon Greyhound Welfare annual show on 11 July. There are a few photos of him in my Flickr Photostream, including a photo of him wearing his gold prize rosette.
Sally and I spent our summer holiday in France and Switzerland, 21 June to 4 July, joining Siân, Tim and Aela for a few days at the Bella Tola campsite near Susten and then staying in a luxury hotel in Grindelwald. We drove there and back through France. The weather was perfect in Susten, over 30 degrees every day. We had a thunderstorm every night in Grindelwald, but it was warm and sunny during the day. I took some great pictures of the Matterhorn and of our mountain walk in the Jungfrau region, which you can view in my Flickr Photostream.
On 17 July we went to a wedding party with a difference. It was called Wedstock and took place in a field in Buckinghamshire. It was modelled on Woodstock, with a number of live bands playing, including Oasis and Madness tribute groups, and we camped overnight in a tent city in the field where the party took place. We had a fantastic time, but it was COLD during the night. Brett helped keep us warm, sleeping with Sally and me in our 1975 retro ridge tent.
Sally and I attended the EUROCALL 2010 conference at the University of Bordeaux, 8-11 September. It was an excellent conference and the food and wine in that region of France are just heavenly! Sally and I ran a workshop on Second Life for beginners, and I was the opening keynote speaker, giving a presentation with the title Where are we now, where have we been, and where are we going?
October 2010: Laparoscopy
On 25 August 2010, I visited Basingstoke Hospital to see Mr Cecil, who gave me the results of the CT scan I had on 2 August. There was evidence of new growth in my abdomen since the previous scan in February, but not at an “alarming” rate. Mr Cecil could not be precise about the nature of the growth – to what extent it was relatively benign growth that could be stripped out easily or whether it was the type that adheres more firmly to the internal organs. The decision was to perform a laparoscopy on 8 October in order to have a closer look. The laparoscopy showed that there is a tumour in the middle of my abdomen, tangled up with the small bowel, the sigmoid bowel and the outside of my bladder, but it appears to be slow-growing. Mr Cecil was of the opinion that performing major surgery at this stage would make me feel a lot worse rather than better and there was no guarantee that he could remove all the cancerous cells. I still feel fit and have a good quality of life, and Mr Cecil said that I could go on like this for years.
November 2010: Interview with my oncologist
An appointment was arranged for me to see Dr Richard Brown, my oncologist, at Wexham Park Hospital on 24 November 2010. He was not in attendance at the oncology clinic, but I did see one of his colleagues, Dr Helen O’Donnell. My consultant surgeon at Basingstoke Hospital, Mr Cecil, had written to Dr Brown, reporting on the results of my CT scan in August and the laparoscopy in October. As often happens, letters sent from Basingstoke Hospital to Wexham Park Hospital had not managed to reach my file at Wexham, but I was able to hand over copies to Dr O’Donnell on the spot. Two missing letters described the results of my last CT scan and my laparoscopy and requested the Wexham oncology team to advise on chemo as a possible way forward. Dr O’Donnell said she could not offer advice on chemo right now as she needed more information, namely copies of my most recent scans at Basingstoke on CD and more detailed information about the laparoscopy. So she said she would write to Basingstoke for this information. At the same time she arranged for me to have another CT scan at Wexham on 8 December and blood tests on 22 December. The oncology team and the surgical team at Wexham would then look at the whole picture, talk to me in early February 2011 and offer advice re chemo to Basingtoke. Dr O’Donnell did, however, point out that chemo is rarely effective in dealing with PMP in general, and there is a lot of uncertainty about the precise nature of my very rare sub-variety (urachal PMP) and how it will react to chemo. As Mr Cecil once said, “Graham, you are a conundrum”.
On the whole Dr O’Donnell was upbeat. She was in agreement with Basingstoke that it was best to intervene with further surgery or chemo only if it is really necessary. She emphasised that PMP is not the same as regular forms of cancer because it tends to stay in one place rather than metastasising and spreading to other organs. It’s not really a cancer – hence the “pseudo” in its name pseudomyxoma peritonei – but it can sometimes become aggressive, behaving like a “real” cancer, and can strangle the bowels, the bladder or female reproductive organs. So, on the whole it’s good news. It’s still a question of watch and wait. My elder daughter Siân accompanied me to see Dr O’Donnell, asked a few pertinent questions and was happy with the outcome. Now Sally and I can relax and look forward to our trip to the Brussels Christmas Market in December and to our family skiing holiday in January 2011.
February 2011: Interview with my oncologist
I got back from our skiing holiday on 29 January. I skied well, although I found it a lot more exhausting than I did when I took up this sport 23 years ago. But, as I approach the grand old age of 69, I suppose I should be grateful that I can still cruise down a mountain safely on two planks clamped to my feet. On 2 February my wife Sally and I had an interview with my oncologist, Dr Helen O’Donnell, who presented me with the results of the CT scan that I had on 8 December 2010 and the blood tests that were carried out later that month. The new growth under my belly button and on the surface of my liver was clearly visible in the scan, but this has not increased substantially since it first showed up in the scan that I had in February 2010. My liver, spleen, gall bladder, stomach, lungs, bladder and prostate all looked OK. Blood tests showed CA125 (46) and CEA (12). Dr O’Donnell’s conclusion was that a policy of watch and wait was still the best option as I have no symptoms of pain or discomfort and I still look and feel fit.
Fifth anniversary of my operation, 1 March 2011
 This is an important landmark for me. Five years ago I could not have imagined I would still be here, especially following the dismal prognosis I was given at the time. I have not been cured and I now have a recurrence of PMP, but I still feel fit and well. During the course of the last five years I have not stopped doing all the things that I enjoy: walking our greyhound every day, playing golf, swimming, travelling, skiing once a year in Austria. We cracked open the champagne!
This is an important landmark for me. Five years ago I could not have imagined I would still be here, especially following the dismal prognosis I was given at the time. I have not been cured and I now have a recurrence of PMP, but I still feel fit and well. During the course of the last five years I have not stopped doing all the things that I enjoy: walking our greyhound every day, playing golf, swimming, travelling, skiing once a year in Austria. We cracked open the champagne!
April 2011: CT scan
I had a CT scan at Basingstoke Hospital on 18 April 2011. The radiologist’s report showed that there had been “moderate growth” since the previous scan at Basingstoke in August 2010. This did not appear to give Mr Cecil, my consultant surgeon, too much cause for concern as his reaction was just to tell me to get in touch with him if I had any problems rather than subjecting me to surgery – which could be quite invasive and would not improve my quality of life. I also had an interview with my oncologist, Dr Richard Brown, at Wexham Park Hospital on 18 May 2011. He did not appear to be too concerned with my condition either, confirming that growth appeared to be very slow. He therefore agreed with Mr Cecil but he thought it would be worthwhile taking a closer look at my last four CT scans, going back to February 2010, to see if growth was consistently slow or speeding up. He advised against chemo as it’s not very effective on my type of cancer and arranged to see me in May 2012. Blood tests carried out in April 2011 showed CA125 (80), CEA (17) and CA19-9 (16).
The summer of 2011
Our summer holiday was virtually a re-run of last year’s holiday. In August 2011 Sally and I drove through France to Switzerland, joining Siân, Tim and Aela for a week at the Bella Tola campsite near Susten and then staying for three days in a luxury hotel in Grindelwald. The weather was variable, mostly warm and sunny, but with a few rainy days. Switzerland was beautiful. Here’s the view from a restaurant in Mürren, where we had lunch.

The summer ended with the EUROCALL 2011 conference at the University of Nottingham, 31 August to 3 September, where I ran a workshop on Second Life for beginners. I picked up some useful contacts at the conference and have been invited to give a presentation at another conference in October 2011.
The results of blood tests carried out in September 2011 showed CA125 (66), CEA (14) and CA19-9 (10) – all down compared to the tests carried out in April 2011 – which sounds like good news! We have booked our skiing holiday in January 2012.
November 2011: Interview with Mr Cecil
My bowels began grumbling with ulcerative colitis flare-ups in March 2011. My GP prescribed Prednisolone, a type of steroid that I have taken many times before. This appeared to bring everything under control by the end of June 2011, and I was able to enjoy the summer. But then I was hit with a major flare-up in early October 2011 and had to start a new course of Prednisolone. My GP thought the flare-up might be connected with an increase of PMP activity and therefore contacted Mr Cecil at Basingstoke Hospital. An appointment with him was arranged for 23 November. Mr Cecil thought that colitis needed to be looked at first and brought into check, so a colonoscopy examination was scheduled for early December. The result showed that I still have moderate colitis and also symptoms of diverticulosis, which is normally treated by watching one’s diet – and this now seems to be working most of the time. So I was able to enjoy a wonderful family skiing holiday in Austria during the last two weeks of January. We had masses of snow. Here is a pic taken from our hotel room in St Johann in Tirol.

February 2012 : CT scan
Since my return from Austria, my condition has deteriorated. I am not sure whether it is progression of the disease or the after-effects of over-indulgence in rich food and booze, combined with the stress of skiing. I had a CT scan on 16 February 2012 that indicated new growth, and it is now obvious that my abdomen is badly swollen.
Sixth anniversary of my operation, 1 March 2012
 Another important landmark! Six years post-op and a wealth of enjoyable years behind me! The downside is that I have a recurrence of PMP that first showed up in a scan shortly before the Fourth anniversary of my operation: March 2010. It’s a slow-grower, but I have now reached the stage where I feel really uncomfortable and I am often in pain, so an appointment has been arranged with Mr Cecil to on 28 March to talk about treatment options.
Another important landmark! Six years post-op and a wealth of enjoyable years behind me! The downside is that I have a recurrence of PMP that first showed up in a scan shortly before the Fourth anniversary of my operation: March 2010. It’s a slow-grower, but I have now reached the stage where I feel really uncomfortable and I am often in pain, so an appointment has been arranged with Mr Cecil to on 28 March to talk about treatment options.
Interview with Mr Cecil, 28 March 2012
Went to Basingstoke today to see Mr Cecil, my consultant surgeon. My last scan (February 2012) shows a mass of ascitic fluid in my abdomen. Mr Cecil thinks surgery is unlikely to be effective and would probably make me feel a lot worse as it would involve the removal of my colon and a segment of my small intestine. This would leave me with a bag round my waist and a nutrition problem resulting from the removal of part of the small intestine. It’s a risky operation and would probably reduce my quality of life significantly. Mr Cecil reckons the fluid can be drained off under local anaesthetic – a procedure known as paracentesis – and that chemo might reduce the hard tumour that is throwing out the fluid. He is writing to Dr Brown, my oncologist, to see what he advises.
Wexham Park Hospital, 3-14 April 2012
So, things turned out to be different from expected. I was admitted via A&E into Wexham Park Hospital (my local general hospital) on 3 April with a suspected bowel blockage. The blockage turned out to be a false alarm, but it was quickly discovered that I had critical anaemia, with a haemoglobin count of 7, and that I had around 8-9 litres of ascitic fluid in my abdomen. Step 1 was to fix the anaemia problem, so I had a blood transfusion of around 600ml. Step 2 was to drain off a substantial amount of the ascitic fluid. It took 5 days to get 3.5 litres out of me – which gave me some relief. I spent a total of 12 days in hospital having all this done, and now I am home. Step 3 is an appointment with Dr Brown, my oncologist, on 18 April. He may advise on further drainage, or he may wish to start with chemo.
Interview with Dr Brown, oncologist, 18 April 2012
I had an appointment with my oncologist, Dr Brown, on 18 April 2012, at Wexham Park Hospital. He was very negative. There was only a very slight chance that systemic chemo would work, he said, as my disease is now at an advanced stage and I am clearly not fit to survive chemo in any case. I should consider myself terminally ill, he said, with maybe weeks or months remaining. Think about organising home nursing care via Macmillan Cancer Support, he said. In the meantime I may need further ascitic draining and more blood transfusions to keep my haemoglobin level above 8. Next step: a second opinion awaited from Dr Rees, the oncologist at Basingstoke.
Interview with Dr Rees, oncologist, 8 May 2012
I had an interview with oncologist Dr Rees at Basingstoke on 8 May 2012. She thought I was too weak to withstand chemo and that the chances of it working on my rare urachal variety of PMP were very slim anyway. She agreed with Mr Cecil that surgery is an unlikely option, as there is very little uninfected small bowel left and if the bad bits were removed then I would have a serious nutrition problem. She was concerned about my distended abdomen and immediately contacted my local hospital, Wexham Park, to arrange ascitic draining on 11 May 2012. The draining procedure went well. I was admitted into the Xray department at 8:30am and by 11:30am the procedure was complete. They managed to drain off 5.5 litres in just three hours and to reduce my weight to 80 kilos! I feel a lot less bloated now, but I am experiencing cramps in my abdomen – due, I guess, to the organs falling back into their correct places now that they have more space!
Macmillan Cancer Support, 25-28 May 2012
Basingstoke Hospital contacted the local branch of Macmillan Cancer Support on my behalf. I was impressed by how quickly they sprang into action. Both my Macmillan nurse and our local district nurse (who liaise with one another and my GP) have visited me during the last few days to assess my needs – medication (especially painkillers), home comforts, financial needs, etc. They are so helpful – and it’s a free service! I feel that at last something positive is being done to make me feel more comfortable. I am now on morphine as a painkiller – very effective. We discovered that my wife can claim state financial benefits as a carer – she has already become an expert in delivering my daily Fragmin injections. I am so impressed by our National Health Service. When it works, it works! My district nurse will call once a week from now on. Today I picked up a 35-pack of Ensure from our local phamacy store. Ensure is a fortified drink that will help me build up my weight – all free, of course! I already feel better!
Thames Valley Hospice, 31 May to 2 June 2012: 70th Birthday BBQ
An eventful week/weekend. On Thursday 31 May and Friday 1 June I received one and a half pints of blood (three bags) to bring up my haemoglobin level, which had dropped to the critical level of 6.6. This was done in the local Thames Valley Hospice, Windsor – lovely place, with excellent facilities. Thames Valley Hospice is more like a 4-star hotel than a hospital: spacious room with electronic bed and easy chair, ensuite bathroom, wifi, flat screen digital TV, unlimited visiting hours – and pets are allowed to visit too. Brett was pleased to see me. On Saturday, 2 June, I was discharged and made my way to my 70th birthdayBBQ at Siân and Tim’s house. Best BBQ I have ever had. We got a friend of Siân and Tim, a caterer, to run the whole show: steak, lamb chops, beefburgers, sausages, chicken, lobster, giant prawns, dips, spicy rice, cous-cous, strawberries and cream. Around 20 guests – all family and close friends. Brilliant day, even through I was a bit shaky after the blood transfusions on the two preceding days.
Thames Valley Hospice, 19 June 2012
Just heard that I will be back in the Hospice for a few days for more blood transfusions and ascitic draining, starting on 19 June 2012.
My diet
I am often asked about my diet. I have not changed my diet since my operation. Sally and I follow the Aphrodite Diet. This is essentially the traditional Mediterranean Diet, one of the healthiest in the world: lots of fresh fruit and vegetables, mainly white meat (red meat once a week), oily fish (salmon, mackerel, herring) and – best of all – a daily intake of red wine, which is a great source of antioxidants. People who live on this diet, especially the red wine drinkers in Burgundy, Bordeaux, Tuscany and Sardinia, suffer less from heart disease and cancer than most other people anywhere in the world. The Sardinians have a very high proportion of fit and healthy people aged over 100 years of age, so they must be doing something right – or maybe they just have a great gene pool. We eat a lot of foods containing antioxidants, e.g. dark chocolate, broccoli, spinach, beetroot, cabbage, sprouts, asparagus, peppers, tomatoes (especially tomato purée), raspberries, strawberries, blueberries and plums. I also eat one banana a day, as bananas are a rich source of potassium – I had a problem with potassium deficiency while I was in hospital in March 2006, and bananas were recommended as a way of building it up. Garlic is great for your health in all sorts of ways – we eat a lot of garlic. See the book, The Aphrodite Diet, by Artemis P. Simopoulos & Jo Robinson http://www.amazon.co.uk/Aphrodite-Diet-Artemis-P-Simopoulos/dp/0091815894. Before and after my operation I took zinc tablets, as zinc is supposed to help boost the body’s ability to heal wounds. I am now taking a daily dose of Manuka Honey and Hemp Oil.
Concluding thoughts
I have not had any chemotherapy as it is claimed that it is not very effective on this type of tumour if administered orally or intravenously. I did not have the Hyperthermic Intraperitoneal Chemo (HIPEC) infusion in my abdomen at the time of my operation on 1 March 2006 as Wexham Park Hospital does not have the facilities to administer it – and (as I have indicated above) the identity of the tumour was only confirmed after the operation. I am assuming that the surgical team did not know precisely what kind of tumour it was until they got it out, and then the initial prognosis was that “it would not be years”.
It is clear that I had a very slow-growing variety of PMP, and it is possible that the tumour took 10-15 years to grow to the massive size that it had reached by the time of my operation. I am now living with a recurrence that raised its ugly head in February 2010, but I battle on regardless – as the Roman poet Horace put it: “Carpe diem!” – “Seize the day!”
I noticed important changes in my health after my operation in 2006. My ulcerative colitis has stayed in remission most of the time, apart from a mild flare-up in February 2007 and a series of more serious flare-ups that started in March 2011. My asthma just seemed to disappear. I no longer have an allergy to shellfish, and I can eat buckets of prawns and mussels with no ill-effects. No one can offer an explanation for all this. Maybe it’s just a case of PMP playing havoc with my immune system over a period of many years, and the removal of the tumour kicked it back into action – but that’s just a guess and not based on medical evidence.
Support of family and friends
Throughout the ordeal following my operation I knew I could rely on my family: my wife Sally, my two daughters Siân and Francesca, my two sons-in-law Tim and Rob, and my brother Chris and sister-in-law Helen. They all visited me while I was in hospital and I appreciated their support. But I was surprised to discover how many really good friends I had: friends who came to visit me in hospital, friends who comforted Sally in my absence, friends who were available as car drivers to ferry Sally to and from the hospital and to take me to follow-up interviews, scans and tests while I was unable to drive. I particularly appreciated the support of friends who had also undergone major surgery and who had survived and were now fit and well. Their encouragement meant a lot to me. I am also grateful to my many friends of different religions who offered their prayers.